Global City Teams Challenge (SmartAmerica)
Date: June, 2014
Collaborators: Harvard University, University of Missouri, MD PnP, DocBox Inc., The University of Pennsylvania, UL, Intel, Talend, RTI, PrismTech, Worcester Polytechnic Institute, Vanderbilt University, DoD / VA, IEEE, Nonnatech, Beth Israel Deaconess Medical Center, NIST

- Sector: Healthcare/Medical
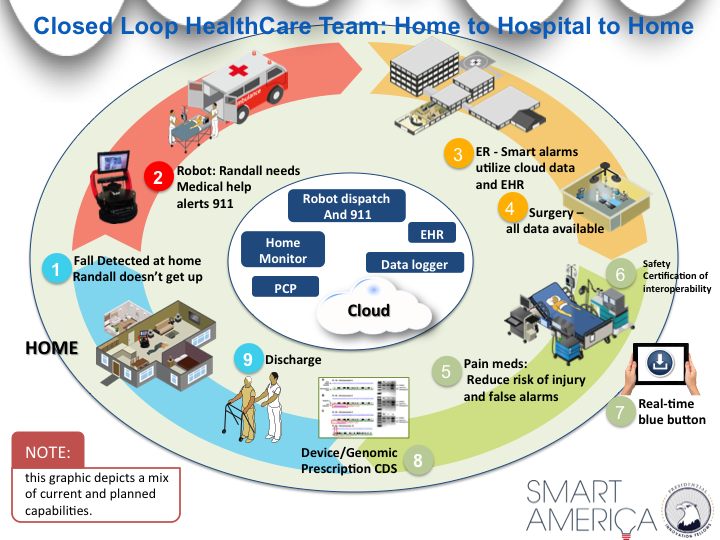
- Scope: Home medical sensors, ambulance, Emergency Room data fusion and closing the loop to home monitoring
- Location: MA
- Timeline: Pilot May/June 2014, Testbed 2014
- Stage: Pilot deployment
- Status: Demonstrated March 2014
- Takeaway: IoT closes the loop for better healthcare outcomes
Closed-Loop Healthcare
Sensor data goes with you seamlessly from home to ambulance to hospital to back home.
Our current healthcare “system” comprises a loose collection of disparate devices and systems that do not connect, or require manual intervention to connect data. This leads to inefficiencies and potentially dangerous conditions due to the lack of interoperability and coordination. Our scenario connects an in-home health monitoring and alert system to interconnected, interoperable components in the hospital to create a cohesive stream of patient-specific health information. We demonstrate the possibilities with our elderly patient, Randall, who lives alone. When Randall falls and breaks his shoulder, a smarthome system detects his fall and sends for help immediately. The history of in-home sensor data helps facilitate personalized and better informed treatment in the hospital. Because the hospital devices and systems are interconnected, Randall receives more coordinated care with lower risk of complications. As Randall transitions between care units, sensor data are automatically delivered to his bedside by the integrated healthcare platform. When Randall returns home, the smarthome system tracks his activity, behaviors, and vital signs with more sensitivity to avoid re-hospitalization. Randall is able to stay in his own home, and his adult children are confident he will receive help if needed. Multiplied across the country, this scenario offers a tremendous potential for cost savings. The Robert Wood Johnson Foundation estimates that we spend $31B annually for preventable hospitalizations among adults. Many could be avoided through better integration and coordination. By streamlining the healthcare operation into a cohesive system, we will save costs, provide better care, and achieve improved health outcomes!
Team Members

Harvard University

University of Missouri

Worcester Polytechnic Institute